
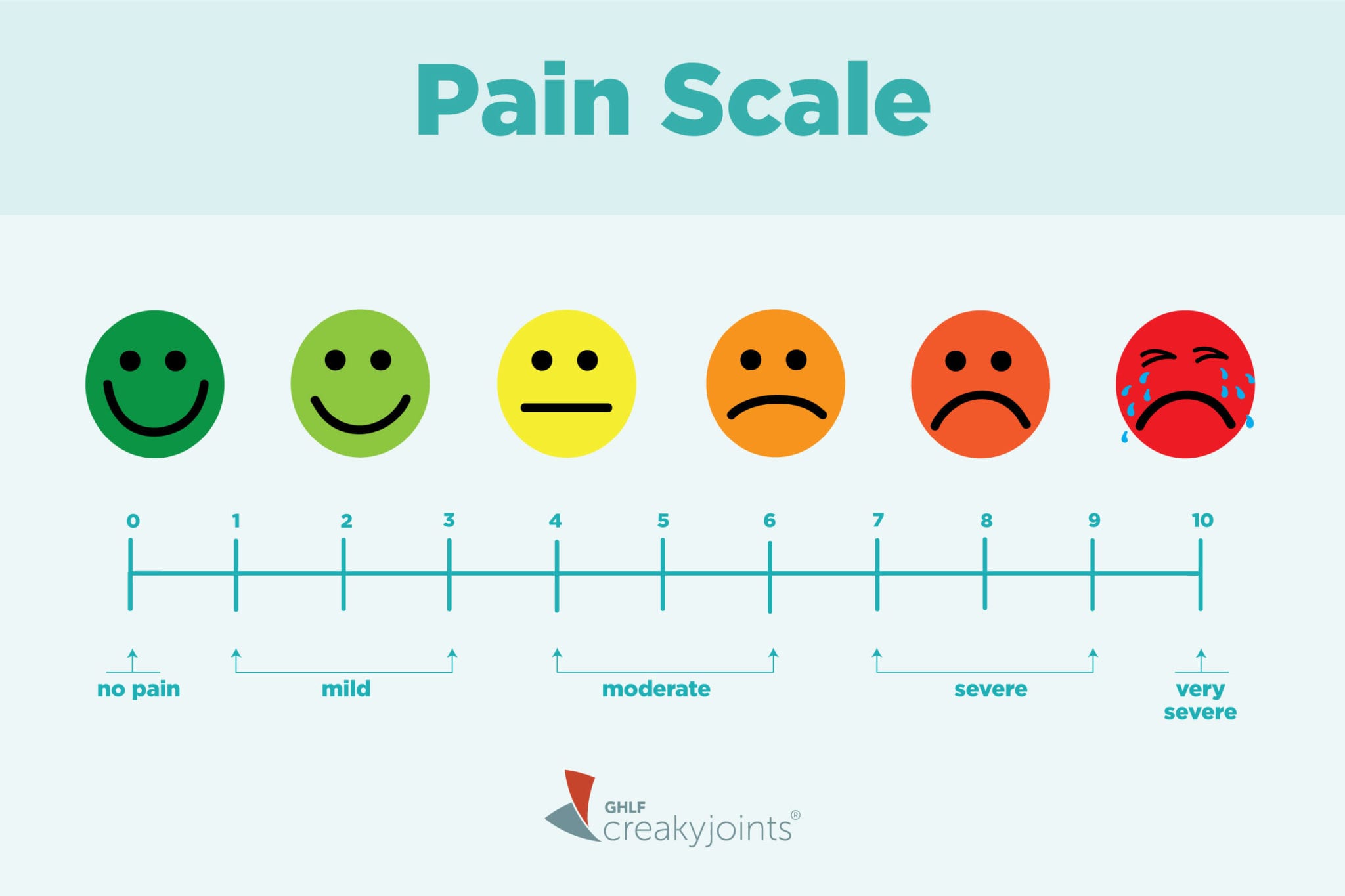
Patients also rate their present pain intensity on a 0 – 5 scale and a visual rating scale. Three pain scores are calculated: the sensory, the affective, and the total pain index. The patient is asked to rate the intensity of each descriptor on a scale from 0 – 3. It consists of 11 sensory (sharp, shooting, etc.) and four affective (sickening, fearful, etc.) verbal descriptors. The SF-MPQ measures sensory, affective–emotional, evaluative, and temporal aspects of pain. The Short form McGill Pain Questionnaire (SF-MPQ) It measures pain interference in seven areas: 1) general activity, (2) walking, (3) normal work, (4) relations with other people, (5) mood, (6) sleep, and (7) enjoyment of life. It can be used to measure worst, least, or average pain over the last 24 hours. The BPI measures pain intensity and the degree of interference with functioning, using a 0 – 10 numerical rating scale. Since chronic pain involves more complex physical, psychological, and social impairments than acute pain, multidimensional measurements – that measure more than just current pain intensity – are recommended. As part of this face rating scale, the child is asked to point to the face that best represents their pain intensity all the way from the face on the left that shows no pain up to the one on the right that shows lots pf pain. The Faces Pain Scale (sometimes called smiley face pain scale) uses six faces to measure pain in children – usually between 3 and 8 years old. While the VAS can be quick to use, it is not as practical as the NRS as it requires clear vision, dexterity, paper, and pen. Like the NRS, the VAS can be used to measure worst, least, or average pain over the last 24 hours, or during the last week. The visual analog scale (also called visual pain scale) or VAS for short, instructs a patient to mark a point on a defined scale to indicate their pain intensity. One can use it to measure pain virtually, or over the telephone. Zero indicates the absence of pain, while 10 or 100 represents the worst possible pain.
It uses a defined scale, and asks patients to verbally give a number to match their pain, place a mark on the number indicating their pain, or even point to the number. The NRS can be used by individuals >8 years old to measure worst, least, or average pain over the last 24 hours, or during the last week. We discuss three: Numerical rating scale (NRS)Īs the name suggests, the NRS uses numbers to rate pain. Face–Legs–Activity–Cry–Consolability (FLACC)Īcute pain can be assessed both at rest and during movement using one-dimensional tools.Assessment of pain in patients with communication problems and in dementia.Measuring cancer pain and pain in palliative care.The Short form McGill Pain Questionnaire (SF-MPQ).visual pain scale, pain chart faces) that clinicians can use to aid their assessment of a patient’s pain, and its related disability. It will provide an overview of commonly recommended measures (e.g. This article is not an exhaustive list of pain measures. children, individuals with cognitive impairment).Įven though measuring pain directly is not possible, there are validated surrogate endpoints that are considered appropriate assessment tools in literature. cancer, back pain, neuropathic pain), and population type (e.g. The recommended pain measure will depend on a patient’s pain duration (acute vs chronic), pain condition and type (e.g. Instead, self-reported measures of pain, disability, and quality of life are recommended. For this reason, objective pain measurement tools are deemed inappropriate to use with patients. A person’s report of their pain experience should be respected, and we cannot conclude on the presence or absence of pain from activity in sensory neurons alone. When measuring pain, we need to remember that pain is always a subjective and personal experience.

Reliable and valid pain measurement is essential to gauging the effectiveness of the treatments we use.


 0 kommentar(er)
0 kommentar(er)
